Follow-up of Serum Creatine Phosphokinase Levels after Ultrasound Guided Suprainguinal Fascia Iliaca Block with Bupivacaine in Total Knee Arthroplasty Patients: An Observational, Controlled Study
By Murat Unal1, Nevzat Gumus1, Nizamettin Guzel2, Serkan Tulgar1, Ersin Koksal3, Mustafa Suren1Affiliations
doi: 10.29271/jcpsp.2024.03.256ABSTRACT
Objective: To determine the myotoxicity of bupivacaine on muscles after suprainguinal fascia iliaca block for postoperative analgesia in total knee arthroplasty (TKA) patients through changes in serum creatine phosphokinase (CPK) levels during the perioperative period.
Study Design: Observational study.
Place and Duration of the Study: Postoperative Recovery Room department of Anaesthesiology and Reanimation, Samsun University, Samsun, Training and Research Hospital, Samsun, Turkiye, between December 2022 and February 2023.
Methodology: Patients undergoing for the procedure of TKA surgery were recruited. (40 controls and 42 SIFIB groups). Serum CPK levels were evaluated preoperatively, at postoperative 6th hour and 24th hour.
Results: From total 82 patients, 42 of them who received SIFIB as a component of multimodal analgesia had serum CPK levels comparable to those in the control group at all time points (p>0.05). While the increase in CPK level at 6th hour relative to baseline was significant in both groups (p<0.05), only the block group demonstrated a statistically significant difference between the 6th and 24th hours (p<0.05).
Conclusion: SIFIB administration did not result in severe bupivacaine-induced myotoxicity in comparison to the control group. SIFIB administration is a safe option when used as part of multimodal analgesia in TKA.
Key Words: Bupivacaine, Creatine phosphokinase, Myotoxicity, Regional anaesthesia.
INTRODUCTION
Regional anaesthesia techniques are increasingly utilised for both surgical procedures and postoperative analgesia.1 Knee arthroplasty is one of the procedures that employs these techniques. Central blocks and peripheral nerve blocks, which were formerly the most popular methods for postoperative analgesia in these patients, are being replaced by facial plane blocks. As the use of ultrasound in regional anaesthesia practice has become more widespread, nerve blocks have become safer, their success rates have increased, and the dose of local anaesthetic drugs has decreased.2
Studies have reported that local anaesthetics injected intramuscularly have a myotoxic effect secondary to inflammation or direct myocyte damage.3 Brun first described this condition in 1959 as a serious complication of peripheral nerve blocks caused by local anaesthetics, and it remains a topic of interest.4 Recent publications on local anaesthetic drug-related myotoxicity have reported an increase in serum creatine phosphokinase (CPK), an enzyme that is predominantly derived from skeletal muscle.5 Myotoxicity could have been directly shown by muscle biopsy, or indirectly by serum glutamate or CPK levels but serum CPK levels are more accessible.
Despite ultrasound guidance, local anaesthetic drugs may be injected into the muscle in the facial plane blocks, or the medicine may leak into the muscle from the facial plane as a result of the high volume administered. This study aimed to investigate the effect of bupivacaine on serum CPK levels in patients who underwent supra inguinal fascia iliaca block (SIFIB) in Total Knee Arthroplasty patients.
METHODOLOGY
This prospective, observational study was conducted in accordance with the Declaration of Helsinki. It was conducted at Samsun University, Training and Research Hospital, Samsun, Turkiye, between December 2022 and February 2023 after local Ethics Committee approval (SUKAEK No: 2022/4/1) and clinicaltrials.gov (NCT05505890) registration.
Patients who underwent TKA surgery under spinal anaesthesia were eligible to participate. American Society for Anaesthesiology Class I-III adult patients aged 18 to 75 were included in enrollment. Exclusion criteria encompassed local anaesthetic drug allergy, bleeding disorder, muscle disease, obstructive sleep apnea, heart disease, liver or kidney, thyroid-parathyroid disease, drugs such as statins that may influence CPK levels, and pregnancy. In order to ensure sample homogeneity, surgical procedures lasting less than 45 minutes or longer than 90 minutes were also excluded from the study.
Patients deemed eligible for the study were divided into two groups based on whether their postoperative analgesia plans included regional analgesia techniques, and analyses were conducted based on these groups.
After standard monitoring and adequate pre-hydration, all patients received a subarachnoid block in the seated position using 12-15 mg of hyperbaric bupivacaine (Buvasin® spinal heavy, Turkiye) with a 25 G quincke-tipped spinal needle from the L4-L5 interspace. If the patient's hemodynamics were stable and the block level was adequate during the control and follow-up, the surgical procedure was initiated.
A standardised perioperative analgesia protocol was administered to patients undergoing knee surgery under spinal anaesthesia in the clinic where this study was conducted. Intraoperatively, just prior to the conclusion of surgery, 1 g (iv) of paracetamol and 25 mg of dexketoprofen were administered. Subsequently, paracetamol was administered every 8 hours and dexketoprofen was administered every 12 hours. A 48-hour elastomeric pump containing 500 mg of Tramadol in 100 mL of saline was connected intravenously to all patients in the recovery room.
Regional anaesthesia techniques have frequently been used for postoperative analgesia. However, they could not be added to multimodal analgesia in all orthopaedic surgeries. These procedures could not be standardised due to issues like the lack of uniformity in the orthopaedic room anaesthesiologist's proficiency with regional anaesthesia techniques and the difficulty in gaining access to the ultrasound equipment and supplies. Therefore, the experienced and competent authors (ST, MU) of this study routinely used this technique in SIFIB, while other colleagues were satisfied with the multimodal analgesia plan mentioned earlier.
Despite these measures, when evaluated by NRS (Numerical Rating Scale), if the patients' follow-up pain scores were >4, 25 mg of meperidine (iv) was given as a rescue analgesic.
Within the first postoperative half hour, following appropriate sterile skin prep of the inguinal region, a supra-inguinal fascia iliaca block was applied using a high-frequency linear transducer (12-18 Mhz, Esaote MyLabTM30 Gold Genoa, Italy), in the postoperative observation unit. The USG transducer was positioned in the oblique plane, superomedial-inferolaterally, just medial to the anterior superior spina iliaca. Sonography identified skin, subcutaneous tissue, the sartorius muscle, the internal oblique muscle (IOM), the iliacus muscle, and the deep circumflex artery. A 21G 85 mm needle (Vygon Echoplex, 85 mm, 21 G, Ecouen, France) was advanced using the in-plane technique from the caudal to the cranial reaching the potential space between fascia iliaca and the iliacus muscle. After confirming needle placement with 1 mL of saline, 50 mL of local anaesthetic containing 0.25 percent bupivacaine (Buvasin®, Turkiye) was injected.
This study's primary outcome was determined to be the CPK level at the 24th hour. The secondary outcome was the number of patients who required rescue analgesia. In addition, the change in CPK levels measured at 6th and 24th hours relative to the baseline value (just prior to surgery) were examined.
Patients' baseline hemogram, BUN, Creatinine, ALT, AST, Electrolytes, Glucose, CPK, and hemostasis profile (aPTT, INR) were evaluated before surgery. In this study, 2 mL of venous blood samples were collected when the patients arrived to the operating room, and six and twenty-four hours after surgery from the antecubital vein, if possible from the arm that did not receive any intravenous fluid-medication (to eliminate any potential variations). The samples were delivered to the laboratory within thirty minutes, and the CPK levels in the blood were analysed immediately. All samples were analysed using a biochemistry instrument of the same brand and model (Beckman Coulter AU5800 model chemistry analyser, United States). CPK levels were measured as U/L in laboratory results, with reference ranges of 10-145 U/L for female patients and 0-171 U/L for male patients.
A pilot study involving five patients per group (SIFIB and control) was conducted. In the SIFIB group, the mean 24-hour CPK was 165.4146.6 U/L compared to 90.670.9 U/L in the control group. Using an alpha level of 0.05, a beta level of 0.10, and a power level of 0.95, 38 participants were deemed to be required for each group. To account for potential dropouts, it was determined that each group had to include at least 40 patients.
Statistical analysis was completed using Statistical Package for Social Sciences (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). The normality of data was determined using the Kolmogorov-Smirnov test. Descriptive data was presented as mean and standard deviation and/or median and interquartile range (25th and 75th percentiles). Comparison of continuous variables was completed with Student’s t-test and ratios was compared using the Chi-squared test. Categorical variables (ASA classification, gender, etc.) were compared using Fisher's exact test and these variables are expressed as number of patients and percentages. ANOVA test was used for repeated measurements to compare the changes in CPK levels between groups and according to baseline. Bonferroni’s correction was made for Post Hoc Analysis. Statistical significance was accepted as p<0.05.
Table I: Patient demographics and laboratory data.
|
|
Control (n:40) |
SIFIB (n: 42) |
p |
|
Age (years) |
65.5±8.48 |
62.5±7.37 |
0.090 |
|
Gender (F/M) |
31/9 (77.5 / 22.5)% |
36/6 (85.7 / 14.3)% |
0.336 |
|
ASA II/III |
32/8 (80 / 20) % |
37/5 (88.1 / 11.9)% |
0.316 |
|
BMI (kg/m2) |
29.63±3.27 |
30.5±4 |
0.278 |
|
Surgery Duration (min) |
52.42±6.63 |
52.83±6.85 |
0.783 |
|
Preop ALT (U/L) |
15.3±6.48 |
18.8±9.38 |
0.050 |
|
Preop AST (U/L) |
20.35±5 |
21.66±8.31 |
0.384 |
|
Preop BUN (mg/dl) |
38.07±14.52 |
34.26±10.91 |
0.185 |
|
Preop Creatinine (mg/dl) |
0.85±0.32 |
0.75±0.17 |
0.106 |
|
ASA: American Society of Anaesthesiology Physical Status Class, BMI: Body Mass Index ALT: Alanine Aminotransferase, AST: Aspartate Aminotransferase, BUN: Blood Urea-Nitrogen t-test is used for age, BMI, Surgery Duration, ALT, AST, BUN, and Creatinine. Chi-square is used for ASA and Gender. |
|||
Table II: Evaluation of baseline, 6th hour and 24th hour CPK values.
|
CPK |
Control Group |
SIFIB Group |
|
||
|
|
Mean score ± SD (95% CI) |
Mean difference |
Mean score ± SD (95% CI) |
Mean difference |
p |
|
Preoperative |
79.17±31.26 (69.17-89.17) |
|
81.07±27.44 (72.51-89.62) |
|
0.771 |
|
Postoperative 6th hour |
94.02±42.69* (80.36-107.68) |
14.85 |
108.52±41.61* (95.55-121.49) |
27.45 |
0.123 |
|
Postoperative 24th hour |
108.17±61.10 (88.63-127.71) |
29.00 |
137.35±97.7* (106.90-167.80) |
56.28 |
0.111 |
|
CPK: Creatine phosphokinase, SD: Standard deviation CI: Confidence interval. |
|||||
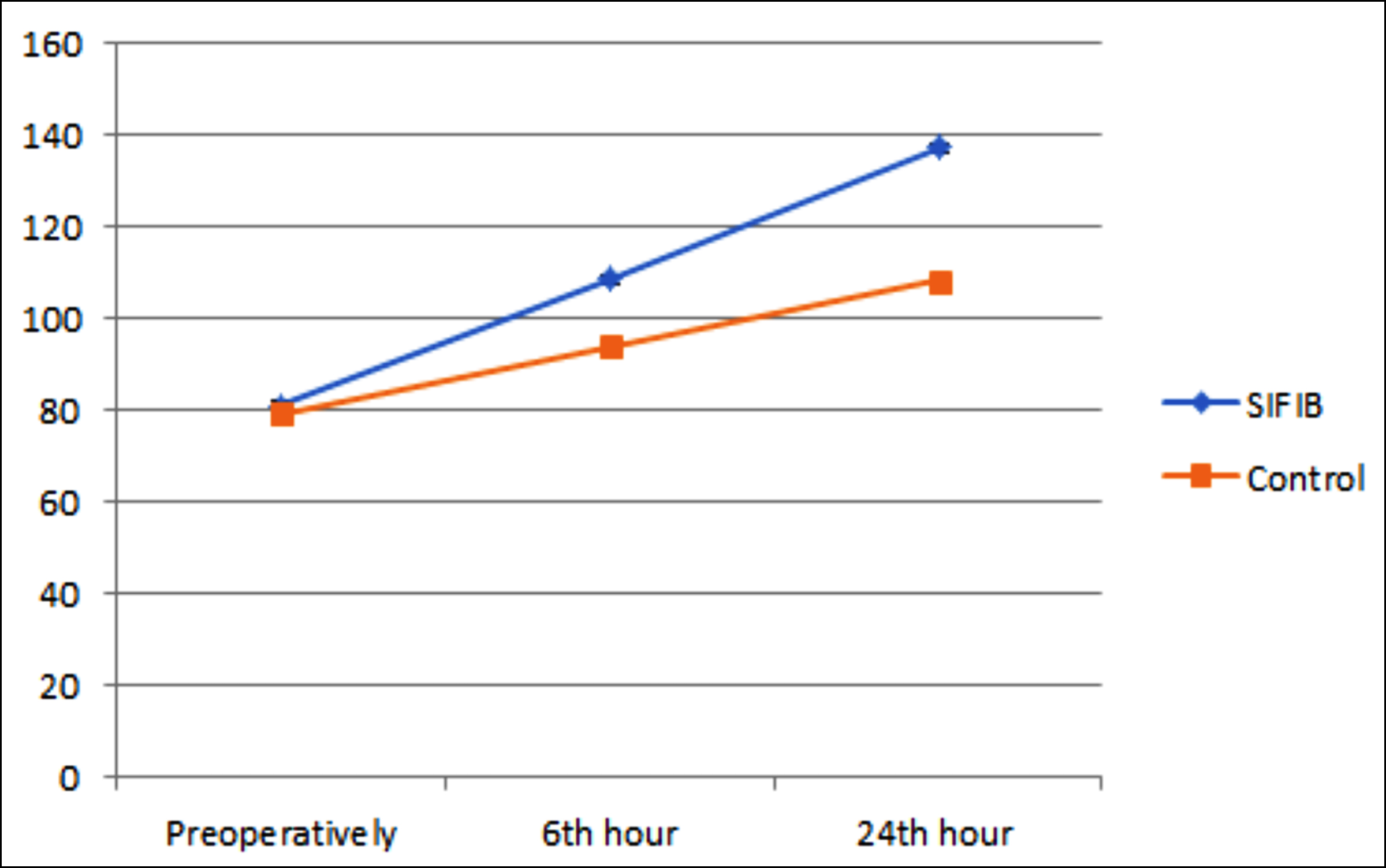 Figure 1: Demonstration of mean CPK levels of groups at baseline, 6th and 24th hour.
Figure 1: Demonstration of mean CPK levels of groups at baseline, 6th and 24th hour.
RESULTS
A total of 85 patients were recruited for the study, with 41 assigned to the control group and 44 to the block group. One patient from each group was excluded from the study because of a delay in the collection of blood samples. One patient in the block group was excluded from the study because the block performance was misinterpreted and approximately 5-7 mL of local anaesthetic was inadvertently administered to the lateral wall of the sartorius muscle.
Comparing the groups based on age, gender distribution, ASA class, surgical time, and preoperative biochemical parameters revealed no statistically significant differences (p>0.05; Table I).
While there was no significant effect of group assignment on the mean changes in CPK levels (F (1, 80) = 2.59, Mse = 5463.78, p=0.111), there was a significant effect of time within groups (F (1.25, 100.05) = 19.16, Mse = 3108, 80, p<0.001). There was not a significant relationship between time and group assignment with respect to the mean changes in CPK levels (F (1.25, 100.05) = 1.96, Mse = 3108.80, p=0.161).
Post hoc tests with Bonferroni's correction revealed a statistically significant increase in the average CPK levels at 6h (p=0.020) compared to baseline in the control group (Table II). However, there was no significant difference between CPK levels at the 6h and 24h time points (p=0.517 and p=0.071, respectively) and at baseline (p=0.517). SIFIB group CPK levels increased significantly from baseline to 6 (p<0.001) and 24 (p<0.001) hours after treatment. CPK levels in the SIFIB group were significantly higher at 24 hours compared to 6 hours (p=0.016). Figure 1 depicts the average upward trend of CPK values by group, and Figure 2 depicts the Box-Plot plot of the quartiles by group.
When stratified by gender, in the control group, none of the nine male patients exceeded the CPK upper limit at 24th hours, whereas seven out of thirty-one female patients did. In the SIFIB group, 9 out of 36 females surpassed the CPK upper limit, compared to half of the 6 males; however, no statistical analysis was conducted due to the limited number of male patients in the sample.
When the groups were compared in terms of the number of patients requiring rescue analgesics within the first 12 hours, 16 patients in the control group and 4 patients in the block group required rescue analgesics and this difference was statistically significant (p<0.05). While the number of patients in the second 12 hours was comparable (9 patients in control group and 7 patients in block group) (p=0.505), the total number of patients requiring rescue analgesic in the first 24 hours was significantly different (18 patients in control group and 9 patients in block group) (p<0.05). The amount of meperidine required for rescue in the control group was 18.12 mg/patient, while in the block group, it was 8.33 mg/patient.
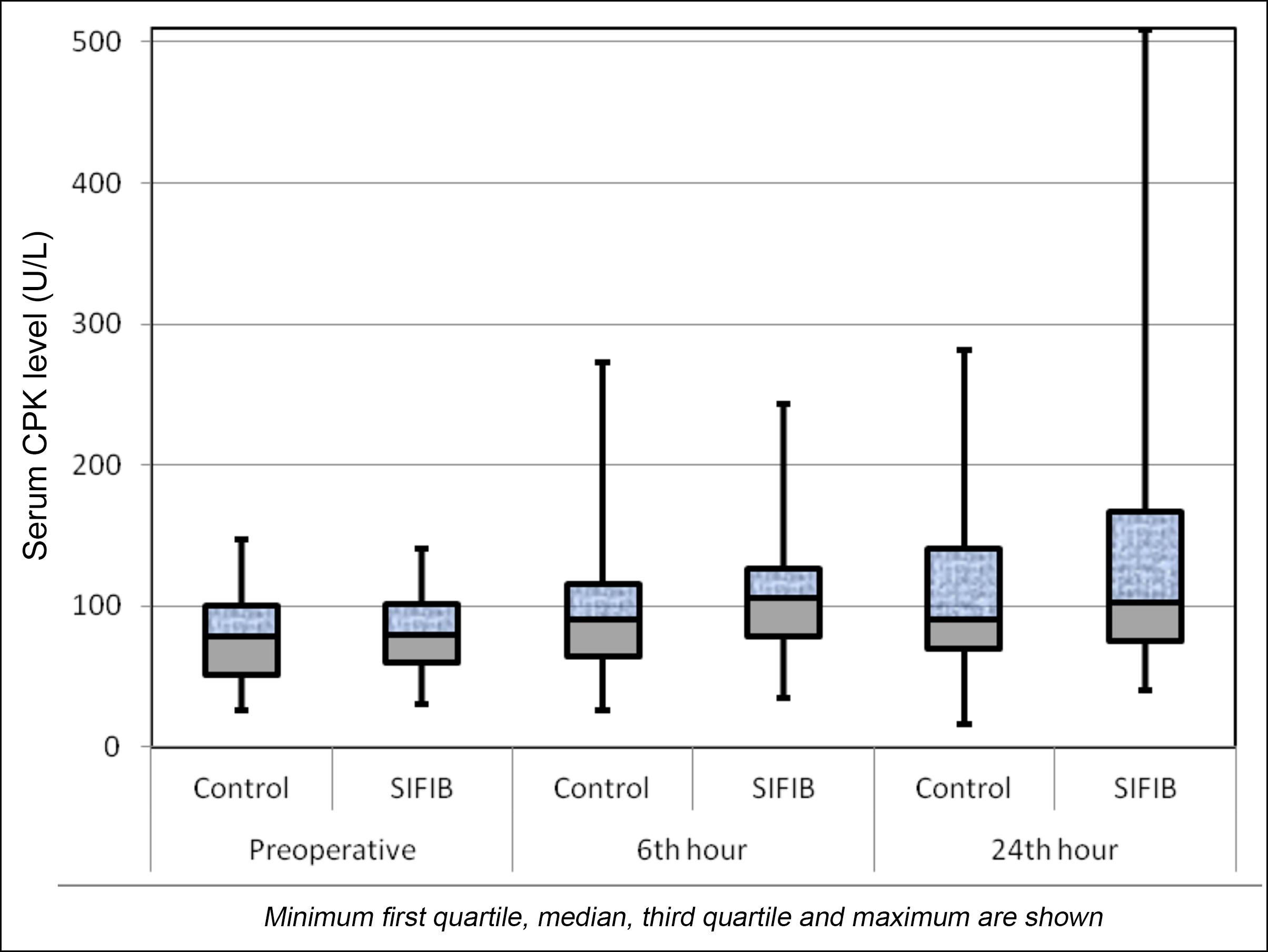 Figure 2: Demonstration of serum CPK levels over time Serum CPK levels (U/L).
Figure 2: Demonstration of serum CPK levels over time Serum CPK levels (U/L).
DISCUSSION
In postoperative analgesia plans for TKA under spinal anaesthesia, comparing SIFIB-containing and control groups showed no significant difference in serum CPK levels at baseline, 6th, and 24th hours. The block group exhibited a statistically significant difference across all time periods, with a steady increase in CPK values. Conversely, the control group only differed between baseline and 6th hour measurements. Additionally, the need for rescue analgesia was higher in the control group.
Interfacial plane blocks enhance postoperative analgesia in multimodal plans.6,7 They have gained popularity in regional anaesthesia, with Bupivacaine being a widely used choice due to its prolonged action and safety.8 Various bupivacaine formulations aim to extend duration, widen confidence intervals, and boost potency, with ongoing clinical studies addressing these aspects.9
Bupivacaine's myotoxicity, neurotoxicity, and chondrotoxicity have been known for years.5,10,11 While local anaesthetic toxicity is a feared complication, myotoxicity is often overlooked. Clinicians employ precautions like imaging, frequent aspiration, and personalised dose-concentration selections to prevent complications.
Local anaesthetics, including bupivacaine, may cause myotoxicity by disrupting calcium homeostasis and affecting mitochondrial function, leading to energy deprivation, reactive oxygen species overproduction, and apoptosis. Human studies indicate myotoxic injury at therapeutic concentrations.12 Despite bupivacaine's reputation for long-lasting effects in anaesthesia, animal studies highlight its specific myotoxic effects, causing rapid cell degeneration in muscle tissue without affecting surrounding structures. Limited cases suggest some potential for muscle tissue regeneration.12,13
Local anaesthetics, even when applied intermuscularly, can cause myotoxicity. Damage is linked to the type, concentration, and duration of exposure, with repeated needle manipulations disrupting fascial planes and causing excessive dispersion.14 Myotoxicity initiates within minutes of contact, leading to months of diffuse inflammation.4
The best indicator of muscle breakdown and myotoxicity is a tissue biopsy, but indirect indicators such as increased serum CPK, increased glutamate, and myoglobunuria are employed in clinical studies.1,15 In this study, serum CPK level measurement was opted, as it is the most accessible and most commonly measured in clinical studies.
Fascial plane blocks involve applying local anaesthetic to interfacial planes, but absorption from these planes and intramuscular spread can occur. Limited studies have explored the neurotoxicity of interfacial plane blocks in humans. Rakhi et al.5 found significantly higher serum CPK levels, indicating myotoxicity, in patients undergoing transversus abdominis plane (TAP) block and PECs-II block compared to the control group. They reported that the elevation in CPK values at the 6th and 24th hours demonstrated statistical significance in both instances. Notably, the increase at the 24th hour was reported to be nearly 63% higher than that observed in the control group. However, there was no significant difference between the block and the control groups (p>0.05). A significant increase at the 6th and 24th hours was seen compared to baseline within the block group, whereas in the control group, the CPK value increase reached significance only at the 6o hour and no significant increase at 24th hour. These differences may be related to the volume of the local anaesthetic agent (bupivacaine) used or attributed to factors, such as the nature of the majority of the surgery. It is a possibility that the potential rise in serum CPK levels may be a result of the significant surgical procedure, such as total knee replacement, and the additional risk associated with bupivacaine is minimal. This study may be repeated for minor surgeries.
Steverink et al. reported another instance of myotoxicity and CPK elevation when bupivacaine was administered intramuscularly to animals in an in-vitro setting.5 In this study, bupivacaine was administered between the muscle and the fascia. The presence of the epimysium might have minimised the contact surface area between the anaesthetic and the muscle tissue, thereby restricting the myotoxic effects associated with bupivacaine.
Published meta-analysis indicates a significant risk of myotoxicity with continuous adductor canal blocks, influenced by variables such as local anaesthetic volume, concentration, and duration.1
SIFIB differs from a true interfacial plane block as it involves injecting local anaesthetic between fascia and muscle tissue, not between two fasciae.16 Due to its contact with muscle tissue, it aligns more with a rectus sheath block than conventional interfacial plane blocks, warranting a distinct evaluation from other regional anaesthetic techniques.
While regional anaesthesia enhances patient recovery, potential adverse reactions may be overlooked. Despite not observing notably high CPK levels in this study (highest values: 508 U/L, 356 U/L, and 354 U/L, all in the block group), it is crucial to acknowledge that unintended intramuscular injections or myotoxicity induced by high volume or concentration can lead to complications like acute kidney injury.17
To minimise local anaesthetic (LA)-induced toxicity, steps include employing the lowest effective concentration, limiting exposure duration, exploring alternative options to prolong the block, carefully assessing high-risk patients, and restricting bupivacaine use in such cases. Incorporating ultrasound-guided peripheral nerve blocks can further reduce administered local anaesthetic. Customising these measures within postoperative analgesia protocols is essential to prevent LA-induced toxicity.5,11,17
This study has some limitations. First, the authors did not utilise randomisation, which may have led to bias. It may be more beneficial to conduct homogenised studies focusing on variables like gender, age, and muscle mass. Considering that the effects of myotoxicity may persist for longer than 24 hours, the authors anticipate that evaluations lasting 48 hours or longer may be more beneficial. In this study, all patients received bupivacaine at a concentration of 0.25%. Minimum effective concentration and volume studies for regional anaesthesia techniques utilised postoperative analgesia will make the clinical environment safer. Similar studies are required for different blocks using various types and concentrations of local anaesthetics.
CONCLUSION
In this study, an increase in serum CPK levels was found when SIFIB was administered with bupivacaine at a concentration of 0.25% under ultrasound guidance; however, this increase was statistically significant when compared to the baseline value, but not when compared to the control group.
ETHICAL APPROVAL:
The study was conducted after obtaining approval from Samsun University Clinical Research Ethics Committee (approval # SUKAEK No: 2022/4/1) and registration on ClinicalTrials.gov Registry (No: NCT05505890).
PATIENTS’ CONSENT:
Informed consent was obtained from all the patients before conducting the study.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
MU: Contributed to data collection, drafted the introduction and discussion, conducted the related literature search, and performed reference settings.
NG: Contributed to the conception and study design, provided critical evaluation, and contributed to the conclusion.
NG: Contributed to the discussion section.
ST: Contributed to the material and methods section, interpreted the data, and conducted the statistical analysis.
EK: Provided critical evaluation of the work.
MS: Contributed to the conception and design of the work.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Hussain N, McCartney CJL, Neal JM, Chippor J, Banfield L, Abdallah FW. Local anaesthetic-induced myotoxicity in regional anaesthesia: A systematic review and empirical analysis. Br J Anaesth 2018; 121(4):822-41. doi: 10.1016/j.bja.2018.05.076.
- Nair AS. Local anaesthetic myotoxicity due to fascial plane blocks: A brief review. Glob J Anesth 2017; 4(1):1-3. doi:10. 17352/2455-203476.000028.
- Zink W, Graf BM. Local anesthetic myotoxicity. Reg Anesth Pain Med 2004; 29(4):333-40. doi: 10.1016/j.rapm.2004. 02.008.
- Brun A. Effect of procaine, carbocain and xylocaine on cutaneous muscle in rabbits and mice. Acta Anaesthesiol Scand 1959; 3(2):59-73. doi: 10.1111/j.1399-6576.1959.tb000 08.x.
- Rakhi V, Kaushal S, Singh S. Measurement of bupivacaine induced myotoxicity in interfascial plane blocks: A randomised controlled trial. Indian J Anaesth 2021; 65 (12):886-91. doi: 10.4103/ija.ija_848_21.
- Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: Back to basics. Reg Anesth Pain Med 2018; 43(4): 341-6. doi: 10.1097/AAP.0000000000000750.
- Ahiskalioglu A, Yayik AM, Celik EC, Aydin ME, Ciftci B, Oral Ahiskalioglu E, et al. The shining star of the last decade in regional anesthesia Part-I: Interfascial plane blocks for breast, thoracic, and orthopedic surgery. Eurasian J Med 2022; 54(Suppl1):97-105. doi: 10.5152/eurasianjmed. 2022.22321.
- Siddiqi A, Mahmoud Y, Secic M, Tozzi JM, Emara A, Piuzzi NS, et al. Mepivacaine versus bupivacaine spinal anesthesia for primary total joint arthroplasty: A systematic review and meta-analysis. J Arthroplasty 2022; 37(7):1396-404.e5. doi: 10.1016/j.arth.2022.03.031.
- Dinges HC, Wiesmann T, Otremba B, Wulf H, Eberhart LH, Schubert AK. The analgesic efficacy of liposomal bupivacaine compared with bupivacaine hydrochloride for the prevention of postoperative pain: A systematic review and meta-analysis with trial sequential analysis. Reg Anesth Pain Med 2021; 46(6):490-8. doi: 10.1136/rapm-2020- 102427.
- Steverink JG, Piluso S, Malda J, Verlaan JJ. Comparison of in vitro and in vivo toxicity of bupivacaine in musculoskeletal applications. Front Pain Res (Lausanne) 2021; 2:723883. doi: 10.3389/fpain.2021.723883.
- Zhang C, Phamonvaechavan P, Rajan A, Poon DY, Topcu-Yilmaz P, Guyton DL. Concentration-dependent bupivacaine myotoxicity in rabbit extraocular muscle. J AAPOS 2010; 14(4):323-7. doi: 10.1016/j.jaapos.2010.05.009.
- Benoit PW, Belt WD. Some effects of local anesthetic agents on skeletal muscle. Exp Neurol 1972; 34(2):264-78. doi: 10.1016/0014-4886(72)90173-2.
- Foster AH, Carlson BM. Myotoxicity of local anesthetics and regeneration of the damaged muscle fibers. Anesth Analg 1980; 59(10):727-36.
- Nouette-Gaulain K, Jose C, Capdevila X, Rossignol R. From analgesia to myopathy: When local anesthetics impair the mitochondrion. Int J Biochem Cell Biol 2011; 43(1):14-9. doi: 10.1016/j.biocel.2010.10.005.
- Cherng CH, Wong CS, Wu CT, Yeh CC. Intramuscular bupivacaine injection dose-dependently increases glutamate release and muscle injury in rats. Acta Anaesthesiol Taiwan 2010; 48(1):8-14. doi: 10.1016/S1875-4597(10)60003-3.
- Kantakam P, Maikong N, Sinthubua A, Mahakkanukrauh P, Tran DQ, Leurcharusmee P. Cadaveric investigation of the minimum effective volume for ultrasound-guided suprainguinal fascia iliaca block. Reg Anesth Pain Med 2021; 46(9):757–62. doi: 10.1136/rapm-2021-102563.
- Dorado-Velasco FC, Loaiza-Ruiz DM. Bupivacaine-induced myotoxicity during a continuous perineural femoral block: Case report. Colombian J Anesth 2020; 48(3):169-73. doi:10.5554/22562087.e908.